Last Updated on April 4, 2025
ACLS Precourse Self Assessment Answers (Pharmacology, Rhythm) Questions Answers 2025. This is a sample copy of the American Heart Association (AHA) Advanced Cardiac Life Support Precourse Self Assessment Question Answers.
Prepare for ACLS certification with our comprehensive 2024 ACLS Pretest Questions and Answers. This full practice test covers all essential topics, ensuring a thorough understanding of ACLS protocols and guidelines.
A perfect resource for healthcare professionals, it’s designed to simulate the actual exam experience with up-to-date content aligned with the American Heart Association’s latest standards. Enhance your skills and confidence for the ACLS certification.
ACLS Precourse Self-Assessment Answers
| Test Name | ACLS Pretest |
| Type of Question | Multiple Choice Question Answers |
| Topics | Pharmacology, Rhythm |
| Total Question | 50 |
| Test Type | Sample / Mock Test |
| Available of Answers | YES |
| ACLS | Advanced Cardiovascular Life Support |
Q1. The most common type of SVT is:
- A. AT.
- B. Ventricular escape rhythm.
- C. AVRT.
- D. AVNRT.
Q2. A 29-year-old man presents with acute altered mental status. His blood pressure is 50/P, ventilations 14 breaths/min. The cardiac monitor reveals PMVT. Your best
course of action in this situation will be to:
- A. Give adenosine rapid IV push.
- B. Give diltiazem IV push over 2 minutes.
- C. Consider sedation and defibrillate immediately.
- D. Perform immediate synchronized cardioversion.
Q3. Examples of irregular tachycardias include:
- A. Sinus tachycardia, accelerated junctional rhythm, and atrial flutter.
- B. PMVT, asystole, and sinus tachycardia.
- C. AFib, atrial flutter, and PMVT.
- D. Accelerated idioventricular rhythm, AFib, and accelerated junctional rhythm.
Q4. Select the incorrect statement regarding vagal maneuvers.
- A. Carotid sinus pressure should be avoided in older patients.
- B. Carotid sinus pressure should be avoided if carotid bruits are present.
- C. An ECG monitor should be used when a vagal maneuver is performed.
- D. Simultaneous bilateral carotid pressure is recommended to ensure slowing of the heart rate.
Q5. Which of the following correctly describes MAT?
- A. In MAT, at least three different P wave configurations are observed.
- B. MAT is an irregularly irregular rhythm with no normal looking waveforms.
- C. Waveforms resembling teeth of a saw or picket fence are observed before each QRS complex.
- D. P waves are uniform in appearance, positive (ie, upright) in lead II, and one precedes each QRS complex.
Q6. A 68-year-old man is complaining of chest pain. His level of responsiveness is rapidly decreasing. His blood pressure is 50/32 mm Hg, his pulse is 230 beats/min, and his ventilatory rate is 6 breaths/min. The cardiac monitor reveals a regular, narrow-QRS tachycardia. Your best course of action will be to:
- A. Defibrillate with 360 J.
- B. Begin immediate transcutaneous pacing.
- C. Sedate and perform synchronized cardioversion with 50 J.
- D. Sedate and perform synchronized cardioversion with 120 J.
Q7. When administering procainamide, the maximum dose is ____ and the maintenance infusion dose is ____.
- A. 0.25 mg/kg, 5 to 15 mg/hour
- B. 0.5 mg/kg, 50 mcg/kg/min
- C. 17 mg/kg, 1 to 4 mg/min
- D. 150 mg, 0.5 mg/min
Q8. A 73-year-old woman is complaining of palpitations and chest pain. Her blood pressure is 72/50 mmHg, her heart rate is 188 beats/min, and her ventilatory rate is 16 breaths/min. The cardiac monitor reveals a wide-QRS tachycardia. Your best course of action will be to:
- A. Defibrillate immediately.
- B. Begin immediate transcutaneous pacing.
- C. Perform synchronized cardioversion with 100 J.
- D. Begin CPR and ventilate using a bag-mask device.
Q9. A 56-year-old woman is complaining of palpitations. When questioned, she denies chest pain or shortness of breath. Her blood pressure is 134/82 mm Hg, pulse 180, ventilations 18 breaths/min. The cardiac monitor shows a regular narrow-QRS tachycardia without visible P waves. Which of the following reflects your best course of action to take at this time?
- A. O2, IV, vagal maneuvers, and adenosine 6 mg rapid IV bolus
- B. O2, IV, vagal maneuvers, and verapamil 2.5 mg slow IV bolus
- C. O2, IV, sedate and perform synchronized cardioversion with 50 J
- D. O2, IV, and atropine 0.5 mg IV every 3 to 5 minutes to a maximum of 3 mg
Q10. A 62-year-old man is complaining of palpitations that came on suddenly after walking up a short flight of stairs. His symptoms have been present for about 20 minutes. He denies chest pain and is not short of breath. His skin is warm and dry; breath sounds are clear. His blood pressure is 144/88 mm Hg, pulse 186, ventilations 18 breaths/min. The cardiac monitor reveals sustained monomorphic VT. An IV has been established. Which of the following medications is most appropriate in this situation?
- A. Dopamine or sotalol
- B. Furosemide or atropine
- C. Nitroglycerin or morphine
- D. Procainamide or amiodarone
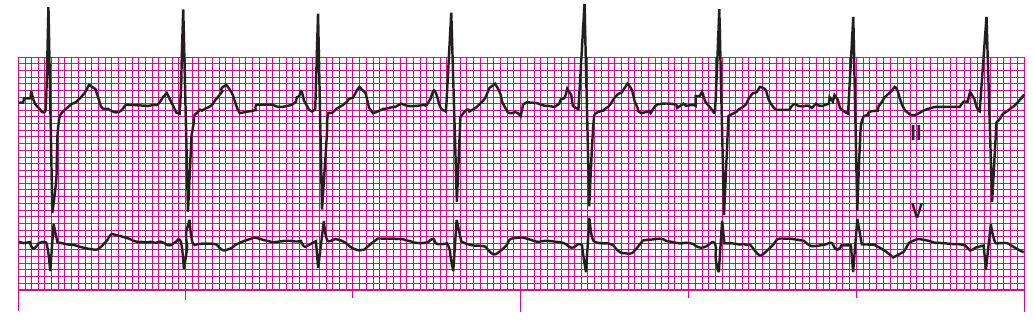
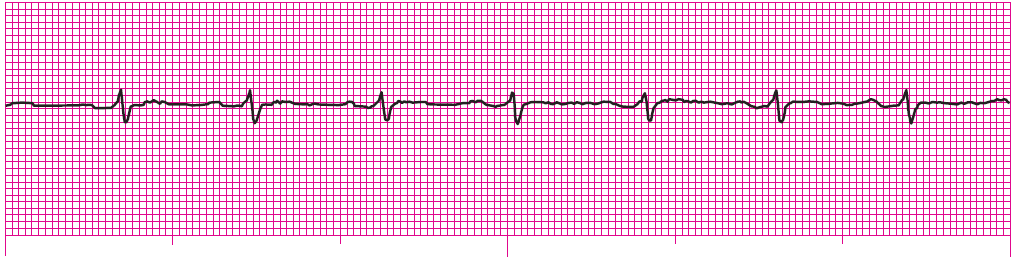
Q11. A shock was delivered as instructed. The cardiologist has arrived. The cardiac monitor reveals this rhythm. What is the rhythm?
Q12. The patient’s vital signs are as follows: Blood pressure: 63/40 mm Hg; heart rate 150 beats/min; and ventilatory rate 20 breaths/min. Breath sounds are clear and equal and his skin is cool, pale, and dry. The patient’s SpO2 on room air is 88%, and he has been placed on the cardiac monitor, which reveals the following rhythm:
Q13. A shock was delivered as instructed. You observe this rhythm on the cardiac monitor. What is the rhythm?
Q14. An ECG rhythm strip shows a regular ventricular rhythm at a rate of 30 beats/min, more P waves than QRS complexes (the P waves occur regularly), a variable PR interval, and a QRS duration of 0.14 second. This rhythm is:
- A. 2:1 AV block.
- B. Third-degree AV block.
- C. Second-degree AV block type I.
- D. Second-degree AV block type II.
Q15. Depending on the severity of the patient’s signs and symptoms, management of slow rhythms may require intervention including:
- A. Defibrillation.
- B. IV atropine.
- C. Synchronized cardioversion.
- D. Vagal maneuvers and/or adenosine.
Q16. With 2:1 AV block, the PR interval:
- A. Is absent.
- B. Shortens.
- C. Lengthens.
- D. Remains constant.
Q17. Which of the following dysrhythmias has the greatest potential for sudden, third-degree AV block?
- A. Junctional rhythm
- B. Sinus bradycardia
- C. First-degree AV block
- D. Second-degree AV block type II
Q18. Which of the following best describes a ventricular escape rhythm?
- A. Rapid, chaotic rhythm with no pattern or regularity
- B. Gradual alteration in the amplitude and direction of the QRS; atrial rate indiscernible; ventricular rate 150 to 250 beats/min
- C. Essentially regular ventricular rhythm with QRS complexes measuring 0.12 second or greater; atrial rate not discernible; ventricular rate 20 to 40 beats/min
- D. Regular ventricular rhythm with QRS complexes measuring less than 0.10 second; P waves may occur before, during, or after the QRS; ventricular rate 40 to 60 beats/min
Q19. With second-degree and third-degree AV blocks:
A. P waves occur regularly.
B. Every other P wave is dropped.
C. P waves are periodically dropped.
D. There are more QRS complexes than P waves.
Q20. TCP may be useful in which of the following situations?
- A. Asystole
- B. Ventricular fibrillation
- C. Sinus tachycardia; blood pressure 108/70 millimeters of mercury (mm Hg), unresponsive
- D. Second-degree AV block type II; blood pressure 64/42 mm Hg, altered mental status
Q21. Which of the following medications increases heart rate by accelerating the rate at which the SA node discharges and by blocking the vagus nerve?
- A. Digitalis
- B. Atropine
- C. Amiodarone
- D. Beta-blocker
Q22. Which of the following best describes third-degree AV block?
- A. Absent P waves, wide QRS, ventricular rate 40 beats/min or less
- B. Rapid rhythm in which the QRS complexes are wide and appear to twist from upright to negative or negative to upright and back
- C. More P waves than QRSs, P waves occur regularly, regular ventricular rhythm, no pattern to PR intervals, QRS narrow or wide
- D. Rapid rhythm in which the QRS complex is wide and usually regular;
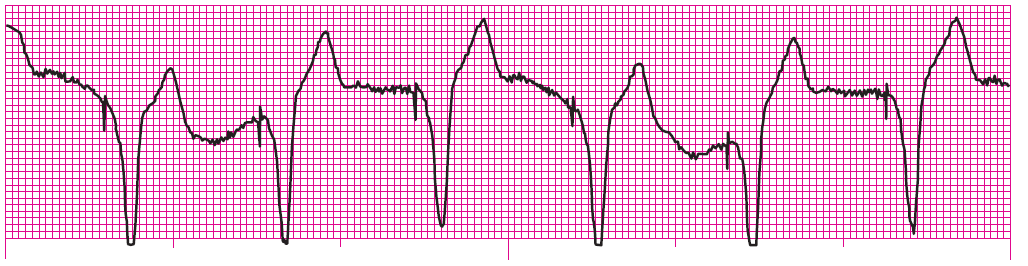
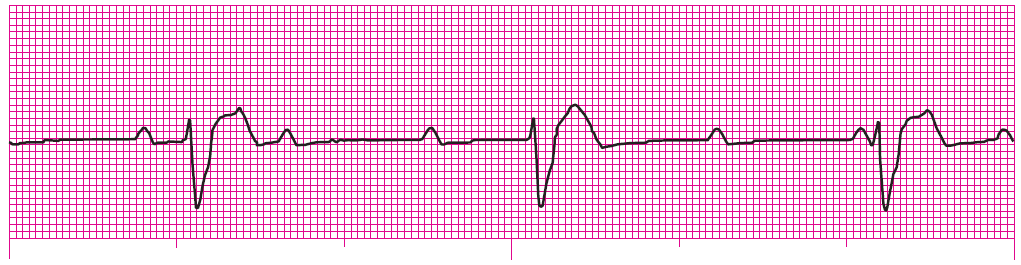
Q23. A 47-year-old man is complaining of dizziness, nausea, and chest discomfort that he rates 4 out of 10. His blood pressure is 74/40 mm Hg; ventilations 16 breaths/min. The patient’s breath sounds are clear. The cardiac monitor displays the rhythm shown.
Recommended treatment for this patient includes:
- A. ABCs, O2, IV, and atropine IV push.
- B. ABCs, O2, IV, and adenosine rapid IV push.
- C. ABCs, O2, IV, and morphine titrated to pain relief.
- D. ABCs, O2, IV, sublingual nitroglycerin, and TCP.
Q24. How would you differentiate a junctional escape rhythm at 40 beats/min from a ventricular escape rhythm at the same rate?
- A. It is impossible to differentiate a junctional escape rhythm from a ventricular escape rhythm.
- B. The junctional escape rhythm will have a narrow QRS complex; the ventricular escape rhythm will have a wide QRS complex.
- C. The rate (40 beats/min) would indicate a junctional escape rhythm, not a ventricular escape rhythm.
- D. The junctional escape rhythm will have a wide QRS complex; the ventricular escape rhythm will have a narrow QRS complex.
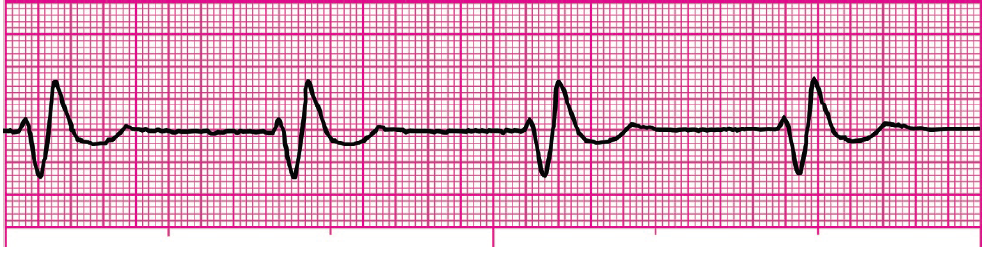
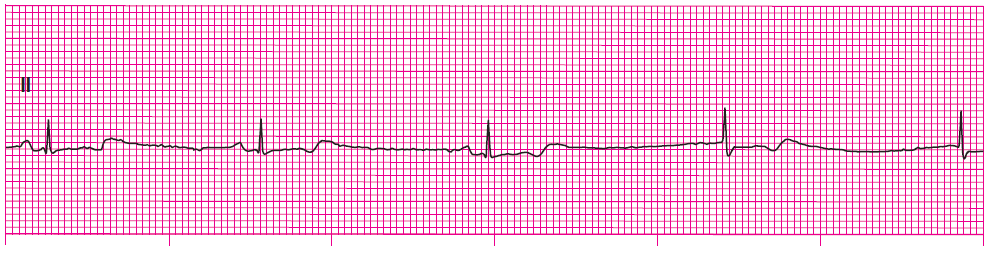
Q25. Identify the following rhythm (lead II):
Q26. Identify the following rhythm (lead II):
Q27. Identify the following rhythm (lead II):
Q28. Identify the following rhythm (lead II):
Q29. Identify the following rhythm (lead II):
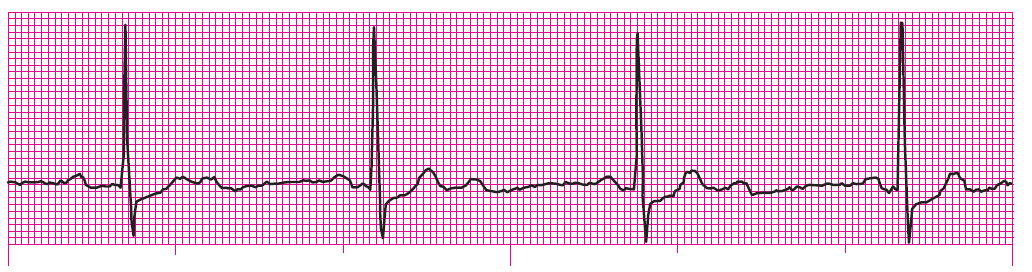
Q30. The patient’s blood pressure is 72/44 mm Hg and his ventilatory rate is 18 breaths/min. Breath sounds are clear and equal and his skin is cool, pale, and dry. The patient’s blood oxygen saturation level (SpO2) on room air is 94% and he has been placed on the cardiac monitor, which reveals the following rhythm:
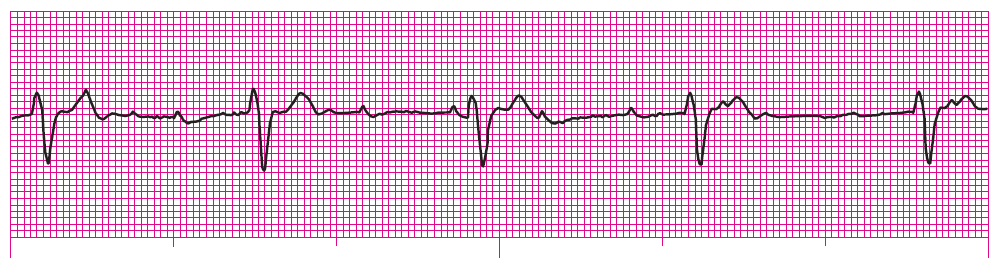
Q31. The patient’s blood pressure is 57/32 mm Hg and his ventilatory rate is 16 breaths/min. Breath sounds are clear and equal and his skin is cool, pale, andmoist. The patient’s SpO2 on room air is 96%. The cardiac monitor reveals the following rhythm: Identify the following rhythm
Q32. Which of the following is the most common cause of the blockage of a coronary artery?
- A. A thrombus
- B. Coronary artery spasm
- C. Coronary artery trauma
- D. Coronary artery dissection
Q33. Beta-blockers:
- A. Increase heart rate.
- B. Decrease the force of myocardial contraction.
- C. Block the conversion of angiotensin I into angiotensin II.
- D. Are contraindicated in patients experiencing an ACS.
Q34. Indicative changes, which are ECG findings that are seen in leads that look directly at the area fed by a blocked coronary artery, are significant when they are seen in two anatomically contiguous leads. Which of the following reflects a pair of contiguous leads?
- A. I and aVF
- B. V1 and V6
- C. V2 and V3
- D. II and aVL
Q35. Which of the following patients is most likely to present atypically with an ACS?
- A. A 34-year-old man with no history of heart disease
- B. A 56-year-old woman with a history of type 1 diabetes
- C. A 65-year-old man with a history of two previous MIs
- D. A 58-year-old man with angina and a strong family history of CAD
Q36. ECG changes characteristic of myocardial ischemia include temporary changes in the:
- A. P wave and ST-segment.
- B. ST segment and T wave.
- C. P wave and QRS complex.
- D. QRS complex and T wave.
Q37. A A66-year-old woman presents in acute distress. She describes a sudden onset of severe chest discomfort and nausea that have been present for 2 hours. An initial 12-lead ECG should be obtained within __ minutes of contact with this patient.
- A. 10
- B. 30
- C. 60
- D. 90
Q38. Which of the following is preferred for the relief of persistent chest discomfort associated with a STEMI?
- A. Aspirin
- B. Morphine
- C. Midazolam
- D. NSAIDs
Q39. Which of the following is (are) the preferred cardiac biomarker(s) for diagnosing MI?
- A. Myoglobin
- B. TnI and TnT
- C. Ischemia-modified albumin
- D. CK-MB
Q40. The recommended initial dose of aspirin is:
- A. 35 to 81 mg.
- B. 81 to 162 mg.
- C. 162 to 325 mg.
- D. 325 to 500 mg.
Q41. A 52-year-old woman is complaining of chest pain. The cardiac monitor reveals a sinus rhythm at 68 beats/min. Her blood pressure is 88/60 millimeters of mercury (mm Hg) and her ventilatory rate is 14 breaths/min. Breath sounds are clear. There are no signs of pedal edema. A standard 12-lead ECG is obtained that reveals 3-mm STE in leads II, III, and aVF. The patient is being given oxygen at 2 L/min by nasal cannula. An IV has been established. You should now:
- A. Give sublingual NTG and aspirin.
- B. Give morphine sulfate and a calcium channel blocker.
- C. Attach right-sided chest leads to rule out RVI.
- D. Give a beta-blocker and determine the patient’s eligibility for reperfusion therapy.
Q42. What is the most common cause of stroke?
- A. A thrombus
- B. An embolus
- C. A ruptured cerebral aneurysm
- D. An arteriovenous malformation
Q43. Paramedics are at the home of a 62-year-old man presenting with signs and symptoms suggestive of stroke. Which of the following is the most important question that should be asked of this patient, family members, or others at the scene?
- A. “When did you last see a physician?”
- B. “When did your symptoms begin?”
- C. “Do you have a history of hypertension?”
- D. “Are you currently taking any blood thinners?”
Q44. Which of the following dysrhythmias is most likely to precipitate a stroke?
- A. Junctional rhythm
- B. Atrial fibrillation
- C. Sinus bradycardia
- D. Ventricular escape rhythm
Q45. A 52-year-old woman presents with a sudden onset of numbness and weakness in her right arm and leg. Family members state her signs and symptoms began while the patient was preparing breakfast 1 hour ago. Examination reveals unequal grips with marked weakness on the patient’s right side. Her blood pressure is 174/86 mm Hg, pulse 88 beats/min, and ventilatory rate 16 breaths/min. Her oxygen saturation on room air is 96%. As you establish vascular access, you note improvement in the patient’s symptoms. After 25 minutes, her grips become equal and there is no weakness on the patient’s right side. You suspect:
- A. Hypoglycemia
- B. Acute ischemic stroke
- C. TIA
- D. SAH
Q46. The acute phase of stroke care:
- A. Includes prehospital care for stroke
- B. Seeks to identify stroke symptoms and stroke type
- C. Is a time-sensitive phase in the first hours after stroke onset
- D. Focuses on confirming the cause of stroke and preventing complications
Q47. During which of the following links of the Stroke Chain of Survival is immediate emergency department triage performed?
- A. Data
- B. Drug
- C. Door
- D. Delivery
Q48. For hospitals that receive acute stroke patients, a patient presenting with a possible stroke should be seen by a physician within __ of his or her arrival.
- A. 5 minutes
- B. 10 minutes
- C. 25 minutes
- D. 45 minutes
Q49. Which of the following must be performed before IV tPA is administered?
- A. Serum glucose
- B. Serum electrolytes
- C. Cardiac biomarkers
- D. Activated partial thromboplastin time
Q50. Fibrinolytic therapy with IV tPA is recommended for selected patients who may be treated within 3 hours of onset of ischemic stroke. Which of the following is a
contraindication to fibrinolytic therapy for this patient?
- A. The patient’s age is 55.
- B. The patient’s symptoms began 45 minutes ago.
- C. The patient has an international normalized ratio of 2.2.
- D. The patient has a history of a myocardial infarction in 1996.
See also:
- Free ACLS Practice Test with Study Guide PDF [2025 Updated]
- ACLS Exam Version A 2023
- ACLS Pharmacology Pretest
- ECG Rhythm Strips Pretest
- ACLS Pretest Questions and Answers 2023
- ACLS Post-Test Answer Key
- ACLS Precourse Self Assessment Answers (Pharmacology, Rhythm)
- AHA ACLS Post-Test Answer Key