Last Updated on April 4, 2025
ACLS Pretest Questions and Answers 2025 (Full Practice Test) ACLS Pretest Questions and Answers 2024 (Free Full Practice Test). You can download this pretest question answer to prepare for the American Heart Association (AHA) Advanced Cardiac Life Support Practice Test exam. Note that this pretest does not represent the actual examination questions.
Prepare for ACLS certification with our comprehensive 2024 ACLS Pretest Questions and Answers. This full practice test covers all essential topics, ensuring a thorough understanding of ACLS protocols and guidelines.
A perfect resource for healthcare professionals, it’s designed to simulate the exam experience with up-to-date content aligned with the American Heart Association’s latest standards. Enhance your skills and confidence for the ACLS certification.
ACLS Pretest Questions and Answers 2025
| Test Name | ACLS Pre-Test |
| Type of Question | Multiple-choice answers |
| Subject | Full SET |
| Total Question | 50 |
| Test Type | Sample / Mock Test 2025 |
| Editable & Printable PDF / Doc | coming soon |
| Available of Answers | YES |
| ACLS | Advanced Cardiovascular Life Support |
1. The drug of choice for most forms of narrow-QRS tachycardia is:
- a. Amiodarone
- b. Atropine
- C. Adenosine
- d. Epinephrine
2. Vasopressin may be used in the management of:
- a. Symptomatic first-degree atrioventricular block
- b. Ventricular fibrillation
- c. Narrow-QRS tachycardia
- d. Atrial fibrillation with a rapid ventricular response
3. Which Of the following could be administered endotracheally if necessary?
- a. Amiodarone, dopamine, procainamide, naloxone, and adenosine
- b. Naloxone, atropine, vasopressin, epinephrine, and lidocaine
- c. Lidocaine, amiodarone, procainamide, vasopressin, and naloxone
- d. Procainamide, epinephrine, lidocaine, adenosine, and dopamine
4. The most common side effects of giving amiodarone are:
- a. Nausea and asystole
- b. Bradycardia and hypotension
- c. AV block and hypertension
- d. Blurred vision and abdominal pain
5. A 75-year-old man has suffered a cardiac arrest. The arrest was not witnessed. CPR is in progress. The cardiac monitor reveals ventricular fibrillation. A monophasic waveform defibrillator is available to you. Your next action will be to:
- a. Deliver three stacked shocks using 200, 300, and 360 joules after 5 cycles (about 2 minutes) of CPR
- b. Give a 2.5- to 5-mg IV bolus Of verapamil over 3 minutes
- c. Deliver a single shock using 360 joules after 5 cycles of CPR and then immediately resume CPR
- d. Give magnesium sulfate 1 to 2 g IV over 10 minutes
6. Which Of the following approaches is recommended during an initial patient evaluation?
- a. Oxygen, IV, monitor
- b. Level Of responsiveness, airway, breathing, circulation, defibrillation if necessary
- c. Temperature, pulse, respiration, blood pressure
- d. Oxygen, IV fluid challenge, vital signs, level Of responsiveness
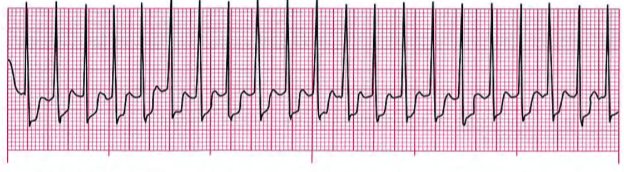
7. A 37-year-old woman is complaining Of shortness Of breath and palpitations. You have placed the patient on oxygen and an IV has been established. Her mental status is rapidly decreasing and she is very pale. Her initial blood pressure was 148/70. It is now 62/38. Breathing is shallow at 8 to 12 breaths/minute. The cardiac monitor shows the following rhythm:
Your best course Of action will be to:
- a. Perform synchronized cardioversion starting with 50 joules
- b. Give sublingual nitroglycerin
- c. Perform CPR for 2 minutes, then defibrillate with 200 joules
- d. Perform CPR and give epinephrine 1 mg IV push
8. At doses recommended for use in cardiac arrest, epinephrine and vasopressin:
- a. Cause significant peripheral vasoconstriction
- b. Neutralize acid accumulated during cardiac arrest
- c. Slow conduction through the atrioventricular node
- d. Cause profound peripheral vasodilation
9. The first antiarrhythmic administered in the management Of the patient in pulseless ventricular tachycardia or ventricular fibrillation is:
- a. Epinephrine or vasopressin
- b. Amiodarone or lidocaine
- c. Vasopressin or amiodarone
- d. Epinephrine or lidocaine
10. During cardiac arrest:
- a. Chest compressions should be interrupted for 2 to 3 minutes to start an IV and insert an advanced airway
- b. Chest compressions should never be interrupted
- c. Interruptions in chest compressions to analyze the ECG, Charge the defibrillator, place an advanced airway, check a pulse, or other procedures must be kept to a minimum
- d. Chest compressions and ventilations should be interrupted every 3 to 5 minutes to permit the members Of the resuscitation team to change positions
11. A 56-year-old woman is complaining Of palpitations. When questioned, she denies Chest discomfort or Shortness of breath. Her blood pressure is 134/82, pulse 180, respirations 18. The cardiac monitor shows a narrow-CRS tachycardia without visible P waves. Recommended treatment for this patient includes:
- a. Airway, breathing, circulation (ABCs); 02; IV; sedation; and synchronized cardioversion with 200 joules
- b. ABCs, 02, IV, vagal maneuvers, and lidocaine 1- to 1.5-mg/kg IV bolus
- c. ABCs, 02, IV, and atropine -mg IV every 3 to 5 minutes to a maximum Of 3 mg
- d. ABCs, 02, IV, vagal maneuvers, and adenosine 6-mg rapid IV bolus
Questions $2 through 16 pertain to the following scenario.
A 78-year-old woman is found unresponsive.
12. From across the room, your first impression Of the patient is that she is not moving, you can see no rise and fall of her chest Or abdomen. and her skin color is pale. When you arrive at the patient’s side, you confirm that she is unresponsive. As you shout for help, your next action in this situation should be to:
- a. Apply the automated external
- b. Open her airway and check
- c. Begin chest compressions
- d. Prepare the to insert an advanced airway
13. If no head or neck trauma is suspected, Which Of the following techniques should healthcare professionals to open the airway?
- a. Jaw-thrust without head tilt
- b. Head tilt-neck lift
- c. Head tilt-chin lift
- d. Tongue-jaw lift
14. The primary survey reveals that the patient is unresponsive and not breathing. A weak pulse is present at a rate of about 70. Your course Of action Will be to:
- a. Begin mouth-to-mouth breathing
- b. Begin ventilating with a bag-valve-mask
- c. Begin chest compressions
- d. Insert an endotracheal tube, Cornbitube. or laryngeal mask airway
15. An oral airway:
- a. May help in the delivery Of adequate ventilation With a device by preventing the tongue from blocking the airway
- b. Is Of proper size if it extends from the tip Ot the nose to the tip Of the ear
- c. Is usually well-tolerated in responsive or semi-responsive patients
- d. Can only be used in spontaneously patients
16. An oral airway is in place. In this situation, the groper rate for bag-valve-mask
- a. 8 to 10 ventilations minute; each ventilation delivered 1 second
- b. 10 to 12 ventilations per minute; each ventilation delivered over 1 second
- c. 12 to 20 ventilations per minute; each ventilation delivered over 1.5 to 2 seconds
- d. 20 to 24 ventilations per minute; each ventilation delivered over 1.5 to 2seconds
17. Which of the following reflects the operation Of a transcutaneous pacemaker for a patient experiencing asymptomatic bradycardia?
- a. The rate should be set between 20 and 60; the current (milliamps) should be increased slowly to maximum Output.
- b. The rate should be Set between 40 and 100; the current should increased rapidly to a maximum Of 160 milliamps.
- c. The rate should be set between 60 and 80; the current should be increased slowly until capture achieved.
- d, The rate should be set between 80 and 100; the current should be increased rapidly to maximum
18. A patient Who presents With a possible (or definite) acute syndrome should receive a targeted history and physical exam and initial 12-Iead ECG within _______ Of patient contact (prehospital) or arrival in the emergency department.
- a. 5 minutes
- b. 10 minutes
- c. 30 minutes
- d. 60 minutes
19. The approximate percentage of oxygen delivered by a simple face mask at 8 to 10 L/min is:
- a. 20% to
b. 40% to
c. 60% to
d. to 100%
20. Most myocardial infarctions occur because of:
- a. Coronary thrombosis
- b. Acute respiratory failure
- c. Coronary artery spasm
- d. Acute volume overload
Questions 21 through 25 pertain to the following scenario.
A 65-year-old woman is found unresponsive and not breathing. You are unable to feel a pulse.
21 . The cardiac monitor reveals the following rhythm.
Which of the following statements is true about this rhythm?
- a. This rhythm is ventricular fibrillation, a “shockable” rhythm
- b. This rhythm is a narrow-QRS tachycardia, a “non-shockable” rhythm
- c. This rhythm is monomorphic ventricular tachycardia, a “shockable” rhythm
- d. This rhythm is a wide-QRS tachycardia, a “non-shockable” rhythm
22. When a shockable rhythm is present during cardiac arrest and a biphasic manual defibrillator is available, the initial energy level selected should be:
- a. 120 joules
- b. 200 joules
- c. 360 joules
- d. The dose recommended by the manufacturer for terminating the rhythm
23. An IV is not in place. The preferred site for initial placement of a large IV catheter is the:
- a. Saphenous vein
- b. Antecubital vein
- c. Subclavian vein
- d. Internal jugular vein
24. Drugs given during cardiac arrest should be given:
- a. By the endotracheal route whenever possible
- b. By continuous IV infusion
- c. By IV bolus and followed with a 20-mL flush of IV fluid
- d. By IV bolus over 2 to 3 minutes and then followed with a 10-mL flush of IV fluid
25. Attempts to establish a peripheral IV have been unsuccessful. Your best course Of action at this time will be to:
- a. Attempt intraosseous access
- b. Insert a central line
- c. Continue peripheral IV attempts until successful
- d. Discontinue resuscitation efforts
26. Amiodarone:
- a. Is given as an initial IV dose Of 300 mg and one repeat dose of 150 mg in cardiac arrest due to pulseless ventricular tachycardia or ventricular fibrillation
- b. Should be given IV or endotracheally in cardiac arrest due to pulseless electrical activity
- c. Is given as a loading dose of 150-mg IV bolus over 10 minutes in cardiac arrest
- d. Should be given only if there is a return of spontaneous circulation after cardiac arrest
27. Rapid heart rates may produce serious signs and symptoms. The physiologic reason for ventricular filling time, which frequently this is that increases in heart rate result in results in stroke volume.
- a. Decreased, decreased
- b. Decreased, increased
- c. Increased, decreased
- d. Increased, increased
28. Dobutamine:
- a. Stimulates alpha, beta-1 , and beta-2 receptors
- b. Is the drug Of choice in the treatment Of symptomatic narrow-QRS bradycardia
- c. May result in asystole when given in high doses
- d. Is given as a 2- to 20-mcg/kg IV bolus
29. A 56-year-old woman presents with a Sudden onset Of chest discomfort that has been present for about 1 hour. The patient describes her discomfort as a “squeezing” sensation in the middle Of her chest. She rates her discomfort an 8 on a O to 10 scale. Her blood pressure is 126/72, respirations 14. Oxygen has been applied, an IV has been started, and the cardiac monitor reveals the rhythm below.
Immediate management Of this patient should include:
- a. Vagal maneuvers and adenosine rapid IV push
- b. Nitroglycerin, morphine, lidocaine Or amiodarone, and aspirin
- c. Aspirin, nitroglycerin, and morphine
- d. Vagal maneuvers and an amiodarone IV infusion
30. Atropine:
- a. Is used to slow the ventricular rate in narrow-QRS tachycardias
- b. Is given in doses of 1 mg to a maximum Of 3 mg in asystole or slow pulseless electrical activity
- c. Is most effective for atrioventricular (AV) blocks below the level Of the AV node
- d. Is given in doses Of 1 to 1.5 mg/kg for symptomatic bradycardia
31. Which of the following statements is true about ventilation with a bag-valve-mask?
- a. A bag-valve-mask device should be equipped with a pop-off (pressure release) valve to overcome increased air resistance in cardiac arrest patients
- b. When an advanced airway is in place, ventilations with a bag-valve-mask must be synchronized with compressions during cardiac arrest
- c. Bag-valve-mask ventilation can produce gastric distention that can lead to vomiting and subsequent aspiration
- d. Bag-valve-mask ventilation can be used only for patients who are not breathing
32. Which Of the following statements is true Of right ventricular infarction (RVI)?
- a. Nitrates, diuretics, and other vasodilators should be avoided in RVI because severe hypotension may result
- b. Typical signs and symptoms Of RVI include hypertension, jugular venous distention, and bilateral rales/crackles
- c. RV infarction or ischemia usually occurs in patients with an anterior wall infarction
- d. Caution should be used when administering IV fluids because the development Of pulmonary edema is increased in patients with RVI
33. Defibrillation is indicated in the management Of:
- a. Asystole and pulseless electrical activity
- b. Pulseless ventricular tachycardia and ventricular fibrillation
- c. Ventricular fibrillation and asystole
- d. Pulseless ventricular tachycardia and pulseless electrical activity
34. Verapamil:
- a. Should be given only to patients with narrow-QRS tachycardia or dysrhythmias known with certainty to be Of supraventricular origin
- b. Is given rapidly as a 2.5- to 5-mg IV bolus (Over 1 to 3 seconds)
- c. Can be safely given to patients with impaired ventricular function or heart failure
- d. Is the drug Of choice for patients with atrial fibrillation or atrial flutter associated with known preexcitation (Wolff-Parkinson-White [WPW]) syndrome
35. Lidocaine may be lethal if administered for which of the following rhythms?
- a. Monomorphic ventricular tachycardia
- b. Idioventricular (ventricular escape) rhythm
- c. Polymorphic ventricular tachycardia
- d. Sinus tachycardia
36. True or False: Side effects associated with transcutaneous pacing are most often related to muscle contraction, pain, and patient intolerance of the pacing stimulus.
- a. True
- b. False
37. A 58-year-old man is complaining of chest pain. Select the question that best evaluates the quality of the patient’s pain.
- a. “When did the pain begin?”
- b. “How wou d you describe your pain?”
- c. “Does anything make the pain better or worse?”
- d. “Where is your discomfort?”
38. Angiotensin-converting-enzyme (ACE) inhibitors:
- a. Increase blood pressure
- b. Increase myocardial workload
- c. May be used in the management of ST-segment elevation myocardial infarction
- d. Include medications such as metoprolol, atenolol, and propranolol
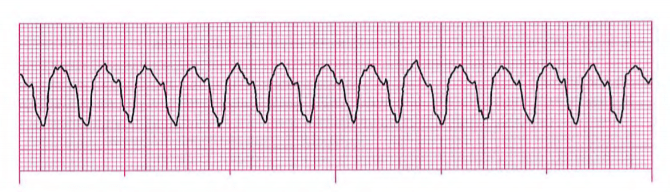
39. A 72-year-old man presents with severe substernal chest pain. His level Of consciousness suddenly decreased as an alarm sounded on the monitor. A quick glance at the cardiac monitor reveals the rhythm below. He now responds by moaning when his name is spoken. His skin is pale and clammy. BP 68/40, R 12. His pulse is weak and fast. Your best course Of action in this situation will be to:
- a. Consider sedation and perform synchronized cardioversion with 100 joules
- b. Start an IV and give a 300-mg dose Of amiodarone
- c. Ask the patient to bear down; if unsuccessful, give adenosine IV
- d. Begin CPR and then defibrillate with 360 joules as soon as a defibrillator is available
40. The most common cause of a stroke is:
- a. A clot (thrombus)
- b. An arteriovenous malformation
- c. A ruptured blood vessel
- d. Spasm Of a cerebral artery
41. True or False: Simultaneous, bilateral carotid massage should be attempted to try to slow the heart rate of a stable patient with a narrow-QRS tachycardia before medication administration.
- a. True
- b. False
42. A 46-year-old woman is found unresponsive, not breathing, and pulseless. The patient’s sister states that 15 minutes ago, the patient said she couldn’t breathe and then lost consciousness. The patient has a history Of congestive heart failure and asthma. CPR is in progress. The cardiac monitor displays asystole. Examination Of the patient reveals no signs of trauma. How should this patient be managed?
- a. Defibrillate once as soon as possible, resume CPR, start an IV, and give epinephrine
- b. Continue CPR, start an IV, intubate using the largest endotracheal tube available, and give epinephrine and atropine
- c. Stop CPR and attempt transcutaneous pacing, then start an IV and begin a dopamine infusion
- d. Attempt synchronized cardioversion using 100 joules; if the rhythm is unchanged, start an IV, and intubate using the largest endotracheal tube available
43. True or False: Rapid, wide-QRS rhythms associated with pulselessness, shock, or congestive heart failure should be presumed to be ventricular tachycardia.
- a. True
- b. False
44. The maximum length of time for a suctioning attempt is:
- a. 10 to 15 seconds
- b. 15 to 20 seconds
- c. 20 to 25 seconds
- d. 25 to 30 seconds
45. Which of the following factors reduces transthoracic resistance and enhances the chance for successful defibrillation in cardiac arrest?
- a. Phase of patient’s respiration
- b. The use of lower energy levels (10 to 25 joules)
- c. Giving calcium chloride before each defibrillation attempt
- d. The delivery of shocks in sets of three when a shock is indicated
46. Successful placement of an endotracheal tube in an adult usually results in the depth marking on the side of the tube lying between the _______ mark at the front teeth.
- a. 15 and 20 cm
b. 16 and 22 cm
c. 19 and 23 cm
d. 20 and 25 cm
47. What is the most common complication in the first few hours of an acute myocardial infarction?
- a. Pulmonary embolism
- b. Hypertension
- c. Ventricular aneurysm
- d. Dysrhythmias
48. Select the incorrect statement regarding the automated external defibrillator (AED).
- a. Some AEDs are programmed to detect spontaneous movement by the patient or others
- b. If a fully automated AED is used and a shockable rhythm is detected, the AED will instruct the AED operator to press the shock control to deliver a shock
- c. Some AEDs have adapters available for many popular manual defibrillators, enabling the AED pads to remain on the patient when patient care is transferred
- d. AEDs will recommend a shock for monomorphic ventricular tachycardia, polymorphic ventricular tachycardia, and ventricular fibrillation
49. Which of the following may be used for rhythm control of acute myocardial in-fraction?
- a. Calcium chloride
- b. Sodium bicarbonate
- c. Lidocaine
- d. Magnesium sulfate
50. Paramedics arrive in the emergency department with a 40-year-old man. When they arrived at the patient’s home, the patient was complaining of a severe chest pain. While taking the patient’s history and vital signs, he experienced a cardiac arrest. The cardiac monitor showed VE The paramedics defibrillated immediately with a successful conversion to a sinus rhythm. The patient responds to a painful stimulus but does not respond to verbal stimuli. His blood pressure is 104/70, respirations 12/min. Which of the following should be done at this time?
- a. The patient’s baseline temperature should be obtained and warming measures should be started until the patient’s temperature reaches 1010 F
- b. The patient should be cooled to 89.60 F to 93.20 F (320 C to 340 C) for 12 to 24 hours
- c. Heat packs should be applied to the patient’s axilla, neck, and groin to prevent hypothermia
- d. Give 50% dextrose in water IV push to make sure sufficient glucose is available for adequate brain function
- Free ACLS Practice Test with Study Guide PDF [2025 Updated]
- ACLS Exam Version A 2023
- ACLS Pharmacology Pretest
- ECG Rhythm Strips Pretest
- ACLS Pretest Questions and Answers 2023
- ACLS Post-Test Answer Key
- ACLS Precourse Self Assessment Answers (Pharmacology, Rhythm)
- AHA ACLS Post-Test Answer Key